Call Us Today! (203) 975-9600
SAME DAY APPOINTMENTS AVAILABLE
December 2022
Tips to Prevent Falls for Adults Over 65
Roughly 1 in 4 older adults fall annually, which is why it is important for people over 65 to practice various safety measures to reduce risks of falling. Exercises can be done to strengthen muscles and improve balance. Pharmaceuticals should be reviewed to eliminate any medicine that causes drowsiness or dizziness. Vision should be checked annually to update eyewear as prescriptions change. Homes should be made as fall-proof as possible by installing grab bars near toilets and in showers and railings on both sides of stairs. Clutter should be eliminated from walkways, bright lighting should be installed, and small rugs should be eliminated or taped down to avoid slippage. A trip to the podiatrist is also recommended for a thorough examination to ensure that feet and ankles are healthy. A gait analysis may also be performed to see if custom orthotics may help improve balance and mobility.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from Preferred Footcare, LLC. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Causes and Symptoms of Plantar Fasciitis
 Plantar fasciitis is one of the most common causes of pain in the heel. This condition can occur when the plantar fascia, which is a band of tissue that runs from the bottom of the heel to the front of the foot, becomes inflamed or torn. Generally, plantar fasciitis is considered to be an overuse injury. There are other issues such as foot biomechanics, ill-fitted footwear, being overweight, or having tight calf muscles that can lead to an increased risk of plantar fasciitis as well. Plantar fasciitis usually results in heel pain that gradually worsens over time, tenderness when pressing onto the heel, and heel pain that is worse in the morning. Patients who notice any of the symptoms of heel pain or plantar fasciitis should consult with a podiatrist for a proper diagnosis and treatment for their condition.
Plantar fasciitis is one of the most common causes of pain in the heel. This condition can occur when the plantar fascia, which is a band of tissue that runs from the bottom of the heel to the front of the foot, becomes inflamed or torn. Generally, plantar fasciitis is considered to be an overuse injury. There are other issues such as foot biomechanics, ill-fitted footwear, being overweight, or having tight calf muscles that can lead to an increased risk of plantar fasciitis as well. Plantar fasciitis usually results in heel pain that gradually worsens over time, tenderness when pressing onto the heel, and heel pain that is worse in the morning. Patients who notice any of the symptoms of heel pain or plantar fasciitis should consult with a podiatrist for a proper diagnosis and treatment for their condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Preferred Footcare, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Do to Keep Your Child’s Feet Healthy
Being a parent involves caring for your child in every way you can. You make sure they are eating the right food, being nice to others, and staying out of any trouble. However, it is also important that you are watchful of their health, more specifically their foot health. Maintaining good foot health in childhood is important in preventing later conditions in life from happening. As children continue to develop, their feet require different techniques of care. Here are some various ways in which you can help your child’s feet stay healthy.
A baby needs a lot of care and attention overall, but the importance of their feet should never be forgotten. Before a baby turns one, their feet change and develop greatly. It is important that during this time, a mother avoids putting tight socks on their child. She should also encourage movement of their feet so the baby can begin to feel more comfortable using them.
As a baby enters the toddler years of his or her life, they are begin to walk around. When your baby begins to take those first steps, it is crucial that they are wearing protective shoes on their feet. As a mother that is observant of your child’s feet, you may notice changes in them. This is completely normal as the feet are becoming susceptible to the activity of walking. It is normal for a toddler to be a bit unsteady or to “walk funny” at first.
When your child grows out of their toddler years, it is important that you begin to show him or her how to care for their feet on their own. Practice with your child proper hygiene in order to prevent foot fungus or infection. Since children are constantly on the move, it is crucial to be cautious of any accidents or injuries that might occur. If an injury occurs, it is advised that you take your child to be examined by a doctor immediately. Since your child is still growing, particular injuries can shift the way in which a bone or other important part of the foot is developing.
Babies and kids are always changing and growing. Your job as a parent is to make sure they stay healthy and making sure they are properly maintained. This involves proper foot care and making sure the feet stay healthy. Following this guide, your child can live a long and happy life.
How to Tell if Your Child May Have a Foot or Ankle Issue
It might be difficult to know when your child has developed a foot or ankle issue. Because they may not be able to verbalize what’s wrong, or their symptoms may be hard to spot, you should keep an eye out for other warning signs. If your child struggles to keep up physically with their friends or their legs or feet get tired, this may be an indication of flat feet. Between the ages of 8 and 14 children may experience sever’s disease, where the Achilles tendon pulls on the growth plate at the back of the heel. This causes heel pain which may cause your child to shy away from physical activities. If your child is hiding their feet from you, they may have noticed some change and want to avoid going to the doctor. If your child seems clumsy or frequently trips or falls it may indicate a balance or neuromuscular issue, or that their feet point inward when they walk or run. Of course if they complain of any pain or discomfort in their feet, or you notice any of these warning signs, make an appointment for your child with a podiatrist for a full examination.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact one of our podiatrists of Preferred Footcare, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
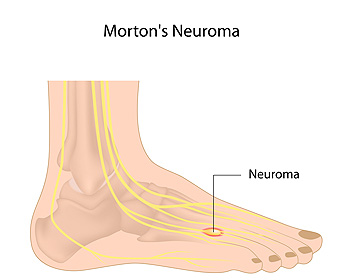
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
What You Should Know About Morton’s Neuroma
Morton’s neuroma is a foot condition in which a nerve in the ball of the foot becomes inflamed. This usually happens to the nerve located between the third and fourth toes. Symptoms of this condition include pain, an achy or burning sensation, numbness, tingling, or prickling that spreads to the toes, and the strange sensation that you're walking on a pebble. It is thought that wearing tight shoes with high heels or pointed toes and repeated trauma to the ball of the foot can increase your risk of developing Morton’s neuroma. The goal of treatment for this condition is to reduce pressure, pain, and swelling, which is often done through footwear and activity modifications, resting and icing the affected foot, and taking anti-inflammatory medications. If you are experiencing the symptoms of Morton’s neuroma, please consult with a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Preferred Footcare, LLC. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Bunionettes: The Pinky Toe Bunions
 You may have heard of bunions, which sometimes pop up at the base of the big toe joint, but what is a bunionette? Bunionettes, also known as tailor’s bunions, are small, bony bumps that occur at the base of the pinky toe joints. Much like regular bunions, bunionettes can be painful, swollen, and red. Finding comfortable shoes that don’t rub up against the affected area may be difficult. Without treatment, bunionettes usually worsen over time. Fortunately, conservative treatments such as wearing wider shoes, a toe spacer, padding, and activity modifications, are often effective in managing the condition. Surgery to correct a bunionette may be beneficial for a smaller percentage of people. To learn more about bunionettes and what treatment methods are best for you, please consult with a podiatrist.
You may have heard of bunions, which sometimes pop up at the base of the big toe joint, but what is a bunionette? Bunionettes, also known as tailor’s bunions, are small, bony bumps that occur at the base of the pinky toe joints. Much like regular bunions, bunionettes can be painful, swollen, and red. Finding comfortable shoes that don’t rub up against the affected area may be difficult. Without treatment, bunionettes usually worsen over time. Fortunately, conservative treatments such as wearing wider shoes, a toe spacer, padding, and activity modifications, are often effective in managing the condition. Surgery to correct a bunionette may be beneficial for a smaller percentage of people. To learn more about bunionettes and what treatment methods are best for you, please consult with a podiatrist.
If you are suffering from bunions, contact one of our podiatrists of Preferred Footcare, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Stamford, CT . We offer the newest diagnostic and treatment technologies for all your foot care needs.